For New Yorkers With Disabilities, Medicaid Expansion Would “Be A Godsend”
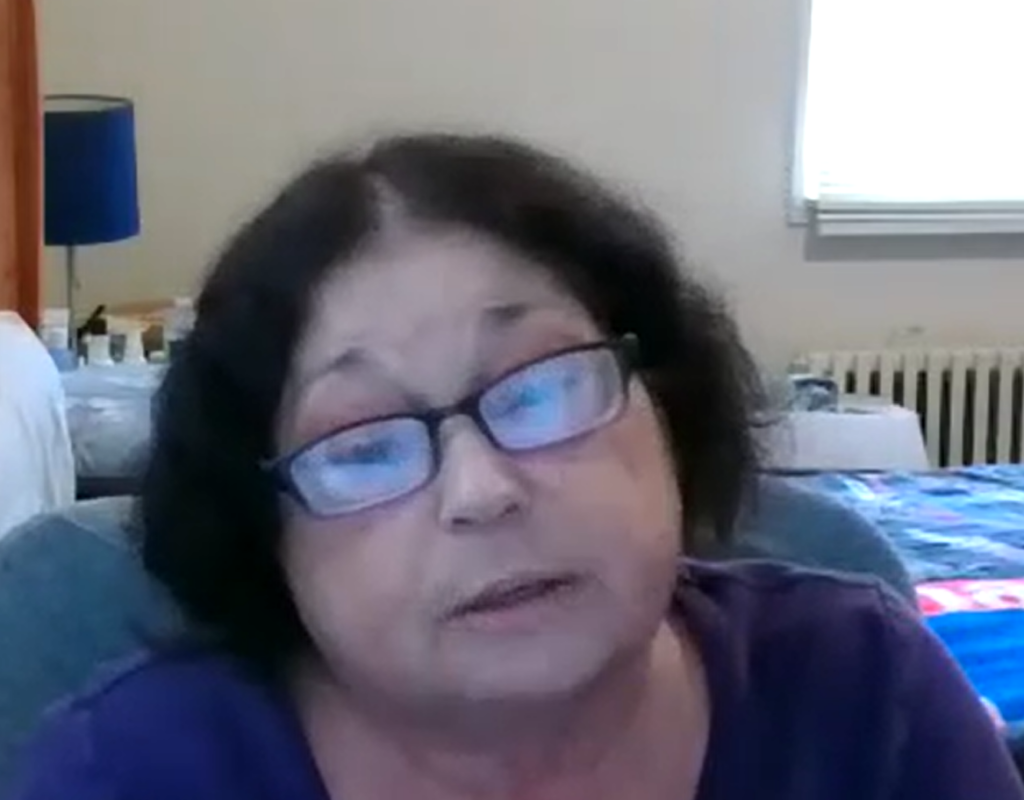
Nancy Rodriguez, a 66-year-old Queens resident, struggles with a number of life-altering cardiopulmonary medical conditions. She works at a doctor’s office despite her disability, to supplement her modest Social Security benefits.
Nancy’s total income is about $30,000 a year, including Social Security — too much to qualify for ordinary Medicaid. Since 2017, she has used the Medicaid Buy-in Program for New Yorkers with Disabilities (MBI-WPD) to cover her medications, multiple specialist visits, and hospitalizations.
Still, Nancy has spent years mired in medical debt. In 2020, her medical bills totaled $500,000, including a 13-day hospitalization for COVID. In 2022 she owed $300,000 for a couple of hospitalizations and a surgery.
“For me to be without health insurance is not acceptable, not even for five minutes.”
Under current law, the MBI-WPD program is limited by income, assets, and age. In her FY2024 Executive Budget, Governor Hochul has proposed expanding the program, so that more New Yorkers with disabilities can work and still qualify for Medicaid coverage.
The Governor has proposed removing the age limit of 65, which Nancy says, “would be a godsend for me.” She does have Medicare, but she does not know how she would manage a Medicare Part B premium, a supplemental “Medigap,” and a drug plan which she figures could amount to $300 per month. “I don’t have that kind of money and I work as many hours as I can. It’s very frightening. I lose a lot of sleep over this.“
We look forward to the passage of New York State’s budget including the expansion of Medicaid Buy-in coverage so that people like Nancy will not have to lose sleep over medical bills and can continue to work. Nancy says, “I am very fortunate that I am able to work and I will continue to work as long as I can do it.”
Let’s keep Nancy working and with critical health coverage.
By Heidi Siegfried, Center for Independence of the Disabled in New York (CIDNY)
The Affordable Care Act increased the income eligibility level for adults without disabilities to 138% of the Federal Poverty Level ($1,563 a month) in 2012. Despite this change, Michael Howard, a 40-year-old man with a mild intellectual developmental learning disability, whose income is $300 a month below the Poverty Level, takes $110 out of his bank account every month and purchases a money order. He mails it to the Medicaid office at the World Trade Center. He does this to keep his Medicaid health coverage. He has been doing this for 7 years.
Why was this happening? Because when the new income eligibility limits were adopted, the “old” Medicaid income eligibility standards ($934 a month in 2022) were retained for people who are in the “Aged, Blind or Disabled” Medicaid eligibility category. Thus, Mike must either incur medical bills in excess of $110 or pay into the Medicaid program to meet his Medicaid monthly “surplus”. Without this he will not have health coverage.
With some savvy budgeting, Mike manages to pay his rent, his cellphone bill, and a $230 cable bill. He shops for the foods he likes but with the increase in food prices, he must, at times, put some items back. His budget cannot accommodate the rising cost of food and his out of pocket medical expenses. He uses four fans instead of an air conditioner because he is worried about the extra electric utility expenses. He says that if he had an additional $110 a month, he would like to save it for a vacation. He would like to visit some more states. He says, “Surplus must go.”
The good news is that the Governor and legislature rectified this discrepancy in the New York State budget that was adopted in April of 2022. In 2023, people with disabilities will have the same income eligibility levels as people without disabilities. This month the New York State Health Department is sending letters to people who have a surplus in the Excess Income (Spenddown) Program telling them how to request a recalculation of their income. And people like Mike will not need to decide between paying for basic needs or medical expenses.



Medicaid Matters New York and Health Care for All New York – the two major statewide health care consumer advocacy coalitions – applaud the State Legislature for several historic additions to the adopted state budget for 2021-22 related to funding for public schools and universities, rental and mortgage assistance, assistance to undocumented essential workers and small businesses, and taking some first steps toward restoring progressivity to the state’s tax system. Millions of low-income New Yorkers who rely on our state’s public health insurance programs will benefit from these improvements to the Governor’s initial set of budget proposals.
However, our State leaders failed to break ground in health care, which is disappointing in light of a decade of austerity budgets and the ongoing nature of the COVID-19 public health crisis. Medicaid Matters and HCFANY are specifically concerned about the following issues:
- The arbitrary Medicaid global spending cap was extended for another year. As a consequence, Medicaid continues to be approached with an austerity mindset. For ten years, Medicaid has suffered from unnecessary cuts, impacting access to services for low-income people, families, people with disabilities and communities.
- Public health insurance coverage was not expanded to low-income immigrants who have had COVID-19. Instead, those who are undocumented remain reliant solely on Emergency Medicaid for acute care and charity care programs for ongoing treatment. As a consequence, many will likely forego seeking necessary care, thereby prolonging illness and suffering, risking death, and incurring medical bills they cannot pay.
- The home care crisis and institutional bias remain unaddressed. Home care workers play a vital role in serving and protecting disabled New Yorkers and seniors living independently, a role that became even more critical and evident during the pandemic. However, New York’s failure to invest in home care has created a “worst in the nation” workforce crisis that prevents meaningful access to home care services for thousands of people and results in greater institutionalization.
- This is the first time in decades that New York State has adopted a discriminatory maternity coverage policy. Instead, only citizen and lawfully residing immigrant women will enroll in free (state-funded) Marketplace coverage after their Medicaid ends—continuing a system that allows for disruptions in care.
- No new initiatives were created to address inequities that are wide-spread throughout our state’s public health, health care, and health coverage systems, despite significant federal pandemic-related funds the state has received over the past year to address these disparities. The pandemic has revealed them clearly, and they can no longer be ignored.
On the positive side, we thank both the Governor and Legislature for these new initiatives:
- Eliminating all premiums in the state’s Essential Plan that provides insurance coverage to low-income people and families who are not eligible for Medicaid. This move will enable them to keep medical, dental, and vision coverage in place without financial barriers, an important step during the ongoing pandemic.
- Protecting the financial stability of community health centers and other safety net providers by delaying the implementation of the planned pharmacy carve-out from the state’s Medicaid Managed Care program.
We also acknowledge and appreciate restorations in funding cuts initially proposed by Governor Cuomo that made no sense given our ongoing pandemic:
- An across-the-board Medicaid rate cut that particularly threatened safety net hospitals that serve large numbers of Medicaid and uninsured patients.
- Elimination of Indigent Care Pool funding to public hospitals.
- Cuts to the state’s Vital Access Provider Assistance Program that keeps certain safety net and rural hospitals financially afloat.
- Additional cuts to Article VI public health funding to New York City.
- Allowing insurers to impose restrictions on the ability of doctors to prescribe certain drugs to Medicaid patients (elimination of the provision known as “prescriber prevails”).
- Another 25% cut to home care workforce recruitment and retention money that would have further harmed community-based long-term care.
- Cuts to programs serving adult home residents.
While as a whole and on the surface it may appear that New York continues to meet the needs of those enrolled in our state’s public health insurance programs and the providers they rely on, the 2021-22 adopted budget fails to make needed investments to turn away from austerity politics, protect all immigrants, expand community-based long-term care, and promote health equity. A lack of harm must not be confused with a budget that provides for what New Yorkers need. We can do better, and we must.
Learn what’s in the HEROES Act from New York’s Congressional leaders and advocates, and find out what you can do get it enacted! The HEROES Act, which already passed the House, would provide much needed pandemic relief and protect the programs, like Medicaid, that are helping people get by during the crisis. Read more here, and register for the virtual rally here.
Action step – Sign-ons needed by close of business tomorrow:
Sign your organization on to this letter (link) drafted by Citizen Action of New York, Medicaid Matters New York, Health Care For America Now, and HCFANY. The letter thanks Senators Schumer and Gillibrand for their work so far to protect New Yorkers during the pandemic – and describes what New Yorkers need included in an enacted version of the HEROES Act. Add your organization’s name here.
Also Coming Up:
100 Years On: Celebrating and Championing Our Civil Rights and Social Programs
So many of our most important civil rights laws and social programs were created in July and August – the National Labor Relations Act (1935), Social Security (1935), the Civil Rights Act (1964), Medicare and Medicaid (1965), the Americans with Disabilities Act (1990). Join fellow New York advocates to celebrate these achievements and fight for justice!
- Dessert Party for Democracy: A Multi-Generational Celebration. We will share pictures and videos of everyday people sharing stories and holding signs saying “I celebrate X because…” We will end with a toast and display of your dessert, holding up signs, including all members of your family or household. August 13, 7:00 – 8:00 PM, register here.
- Renewing the American Promise: Defending and Expanding Our Social Contract. Learn more about the civil rights and social programs that everyday New Yorkers benefit from and learn how these programs and laws are at risk. August 19, 12:00 – 1:00PM, register here.