The season of giving is coming early for many New Yorkers seeking hospital care this year. As of last month, amendments to New York’s Hospital Financial Assistance Law (HFAL) will make it easier to apply for and cover more patients under financial assistance programs. The HFAL, also known as Manny’s Law, was implemented in 2006 in response to the death of Manny Lanza, 24. Lanza passed away after being denied life-saving surgery due to his uninsured status.
Financial assistance programs help many patients receive affordable care on a sliding fee scale based solely on their household income. This includes patients who are uninsured or those with insurance, but medical costs are a big strain on their income. Rising hospital prices in recent years have left many patients unable to afford the care they need, often leading them to incur medical debt. A 2023 Urban Institute reported that 740,000 New Yorkers had medical debt, with nearly half of them owing $500 or more. This updated HFAL will streamline the process and expand the eligibility of hospital financial assistance. New Yorkers will finally be able to have some more relief from medical debt and rising healthcare costs.
The following changes will be made to HFAL and medical debt in New York.
- All hospitals licensed by the New York State Department of Health (NYSDOH) are required to use a Uniform Hospital Financial Assistance form and inform patients of financial assistance availability in writing during registration and at discharge (regardless of the hospital’s participation in the Indigent Care Pool). Eligibility will not consider the patient’s immigration status. Before this amendment, many patients were never informed financial assistance existed and many hospitals requested information that was not legally required, like Social Security Numbers or tax returns, which often scared patients away from applying.
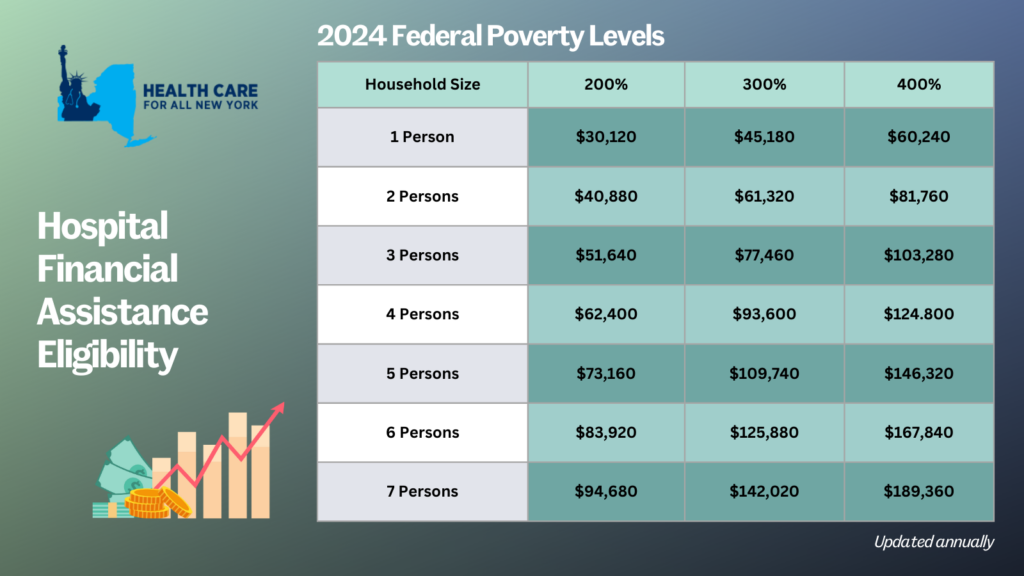
- Patient eligibility for financial assistance will be expanded for those uninsured and underinsured. Under the new law, being underinsured is defined as patients whose paid medical expenses, excluding insurance premiums, exceeds 10 percent of their income within the last 12 months. Uninsured patients will now qualify if their household earns up to 400 percent of the federal poverty level (FPL) and will receive free or discounted care based on a sliding scale (see the table below for eligibility guidelines based on household size and the payment sliding scale). These guidelines will be solely based on the FPL and are updated through the Poverty Guidelines | ASPE.
- Individuals can now apply for hospital financial assistance at any time.
- Hospitals may not sell patients’ debt to third party entities like debt collection agencies. Often these agencies use aggressive and threatening practices to make patients pay medical debt.
- Hospitals are prohibited from bringing lawsuits against patients earning up to 400 percent FPL to collect unpaid medical bills. And lawsuits to collect unpaid balances cannot be brought until 180 days after the first medical bill. Lawsuits have disproportionately affected people of color and low-income residents. For example, according to a 2024 Community Service Society of New York report, over a third of lawsuits filed by State-run hospitals were filed against patients who lived in zip codes where residents are disproportionately people of color. Additionally, nearly all these cases were filed against patients that should have been eligible for hospital financial assistance.
- To measure this impact, hospitals will report to the DOH the number of people that have applied for financial assistance annually including age, gender, race, ethnicity, and insurance status.
With this series of reforms, more New Yorkers will be able to receive affordable hospital care and reduce their chances of incurring medical debt. The HFAL was a landmark reform back in 2006 and has been far improved with these amendments.
Here’s a copy of the form hospitals must use now.
If you need assistance in applying for hospital financial assistance, contact Community Health Advocates at 888-614-5400.
Between 2015 and 2019, New York’s hospitals sued 40,000 New Yorkers who could not pay their medical bills. Hospitals were unable to file new lawsuits against patients for a couple of months during the pandemic. However, a quick look at just the most litigious hospitals shows over 500 cases filed since courts starting accepting civil cases again.
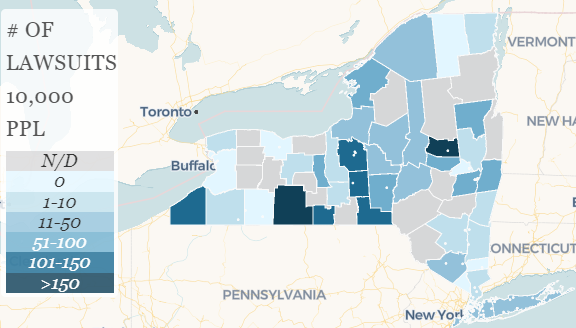
A new map from the Community Service Society (with help from BetaNYC) shows where residents are most likely to be sued by their hospital. Residents of Fulton and Steuben County – areas where patients lack many choices about hospital care – are most frequently sued. In the New York City area Nassau, Suffolk, and Queens County residents are most frequently sued.
What can we do?
- Read the original report, which provides more data on the lawsuits, which hospitals filed them, how it impacts health equity, and describes measures that New York could take to stop these abuses.
- Tell your legislators to stop hospitals and debt buyers from taking collection actions against patients during the pandemic. S8365/A10506 would achieve this and more: it would stop interest from accruing on medical debt during the pandemic, permanently cap interest rates on medical debt at the U.S. Treasury rate from the current 9 percent, extend grace periods for insurance premiums, and stop late fees or credit agency reports against members who pay late premiums.
- Take action on CSSNY’s End Medical Debt campaign and increase support for the Patient Medical Debt Protection Act. The Patient Medical Debt Protection Act was introduced before the pandemic and already has with 34 sponsors in the State Assembly (A08639) and 18 sponsors in the State Senate (S06757). This bill does more to make hospital billing fairer for patients, including requiring a standardized itemized bill and stopping hospitals from charging unfair facility fees that are not covered by insurance.
There is an urgent need for New York to protect patients from unfair billing practices, and the Patient Medical Debt Protection Act does just that: We can’t take another 40,000 patients being sued before we fix this problem.
New York State’s budget included harmful changes to Medicaid – though many of those changes are delayed (see our joint statement with other Medicaid advocates here). The Medicaid cuts are going to be an on-going issue throughout the year. But outside the Medicaid budget, there were a few wins for consumers.
Full Funding for Consumer Assistance Programs
New York’s consumer assistance programs received full funding. These programs include the Community Health Advocates and the Community Health Access to Addiction and Mental Healthcare Program (CHAMP). Both programs provide free, independent help to make sure your health insurance works and that you can access care. Both are running full speed ahead despite social distancing – if you ever need help dealing with care denials or prior authorizations or even finding a doctor, give them a call! You can find more info about the Community Health Advocates here, and about CHAMP here.
Other good CHAMP news – the budget created a fund to make sure that people who need assistance getting mental healthcare or addiction help can get the services they need. The fund will be filled using fines against health plans that do not follow the rules about ensuring access to those services. New York has had parity laws for a long time that require plans to treat mental healthcare the same as other healthcare – the fund will help hold plans accountable while providing resources to people who need care.
Protecting Patients from Medical Debt
Two parts of the Patient Medical Debt Protection Act made it into the budget (learn more about medical debt in New York here). One reduces the statute of limitations for medical debt court cases from six years to three. After six years, most people don’t have the same insurance or the records they need to defend themselves against hospitals in court. The budget changes the law so that these cases must be filed sooner, giving defendants a better chance to defend themselves. The second change closes a loophole in the state’s surprise medical billing law – now emergency charges by either the hospital or individual providers will be covered by the law. That means fewer unanticipated and unfair bills.
Making Prescription Drugs More Affordable
There were two actions on prescription drugs in the final budget. First, the budget caps co-pays on insulin at $100 every 30 days. There’s a lot more the state could do on prescription drugs (see S6492/A8533) but this will be a big help to people with insurance who depend on insulin. The budget also creates a drug accountability board that will help the Commissioner of Health investigate prescription drug price gouging.
Fair Hospital Funding
Finally, the enacted budget ends the transition collar for the state’s indigent care pool. The transition collar was part of a system that short-changed safety net providers and rewarded hospitals that provide little or no financial assistance to patients. Advocates have worked for years to improve how indigent care pool funds are distributed – and won some improvements six years ago. When the funding formula changes happened, the state instituted a transition collar to slowly phase them in. But the transition was extended every year – until now. Without it, New York will finally fully implement the formula improvements and move closer to a fair system. You can learn more about the indigent care pool and its history here.
By Bob Cohen, Policy Director, Citizen Action New York
The COVID-19 pandemic is exposing just how broken the US health care system is, including our inability to control disease outbreaks when many people simply cannot afford basic medical care. Patients should never fear seeking medical care because of cost, but for many New Yorkers that is the reality. And a new report by the Community Service Society highlights one of the worst outcomes for patients who cannot pay their medical bills – lawsuits filed against them by the hospitals they turned to for help. The report, “Discharged Into Debt,” finds that New York hospitals have filed over 30,000 debt collection lawsuits in the past five years. The study only looked at hospitals in 26 of New York’s 62 counties – which means the actual number of lawsuits is much higher.
New York State’s non-profit hospitals have a social mission. Legally, they are charities that pay no federal, state or local taxes and receive a total of $1.1 billion each year from the ICP. As a condition for receiving this funding, hospitals are required to offer financial assistance to patients without insurance.
The report, based on an examination of the New York State Ecourts public database and a sample of hundreds of individual case files, documented a number of abusive practices by New York hospitals. For example, hospitals claimed in legal papers that they were entitled to payment for unspecified items like “miscellaneous” and “ancillary procedures” charges. And, because New York allows hospitals to charge an outrageous 9% interest rate on outstanding bills and to tack on court fees on top of that, the median amount the hospital sued on was $1,900 but the median judgment amount was $2,300. In many cases, hospitals sued patients that were eligible for financial assistance without offering it, as required by law.
The report also found large racial disparities in the treatment of patients that owe medical debt, particularly upstate. In counties like Onondaga (Syracuse), Monroe (Rochester), Albany and Erie (Buffalo), a much higher proportion of people were referred to collections for medical debt in communities of color than white communities.
And, the study documents, patients were almost always totally outmatched by large collection law firms retained by the hospitals. Process servers often illegally serve relatives or co-tenants instead of patients, violating basic provisions of the U.S. constitution and in state laws designed to make sure people have reasonable notice of lawsuits so they can adequately defend themselves. And, 97% of the patients in the study were unrepresented and didn’t even attempt to respond to the lawsuit. The result is often wrecked credit, and unpaid judgments that threaten the financial futures of consumers and their families.
The CSS report adds to the case for passage of the Patient Medical Debt Protection Act (A.8639/S.6757), which addresses some of the most egregious medical billing practices. Fixing these practices, including lawsuit abuses, is a critical step in fixing our broken health care system and making health care affordable to low and moderate income New Yorkers.

