The season of giving is coming early for many New Yorkers seeking hospital care this year. As of last month, amendments to New York’s Hospital Financial Assistance Law (HFAL) will make it easier to apply for and cover more patients under financial assistance programs. The HFAL, also known as Manny’s Law, was implemented in 2006 in response to the death of Manny Lanza, 24. Lanza passed away after being denied life-saving surgery due to his uninsured status.
Financial assistance programs help many patients receive affordable care on a sliding fee scale based solely on their household income. This includes patients who are uninsured or those with insurance, but medical costs are a big strain on their income. Rising hospital prices in recent years have left many patients unable to afford the care they need, often leading them to incur medical debt. A 2023 Urban Institute reported that 740,000 New Yorkers had medical debt, with nearly half of them owing $500 or more. This updated HFAL will streamline the process and expand the eligibility of hospital financial assistance. New Yorkers will finally be able to have some more relief from medical debt and rising healthcare costs.
The following changes will be made to HFAL and medical debt in New York.
- All hospitals licensed by the New York State Department of Health (NYSDOH) are required to use a Uniform Hospital Financial Assistance form and inform patients of financial assistance availability in writing during registration and at discharge (regardless of the hospital’s participation in the Indigent Care Pool). Eligibility will not consider the patient’s immigration status. Before this amendment, many patients were never informed financial assistance existed and many hospitals requested information that was not legally required, like Social Security Numbers or tax returns, which often scared patients away from applying.
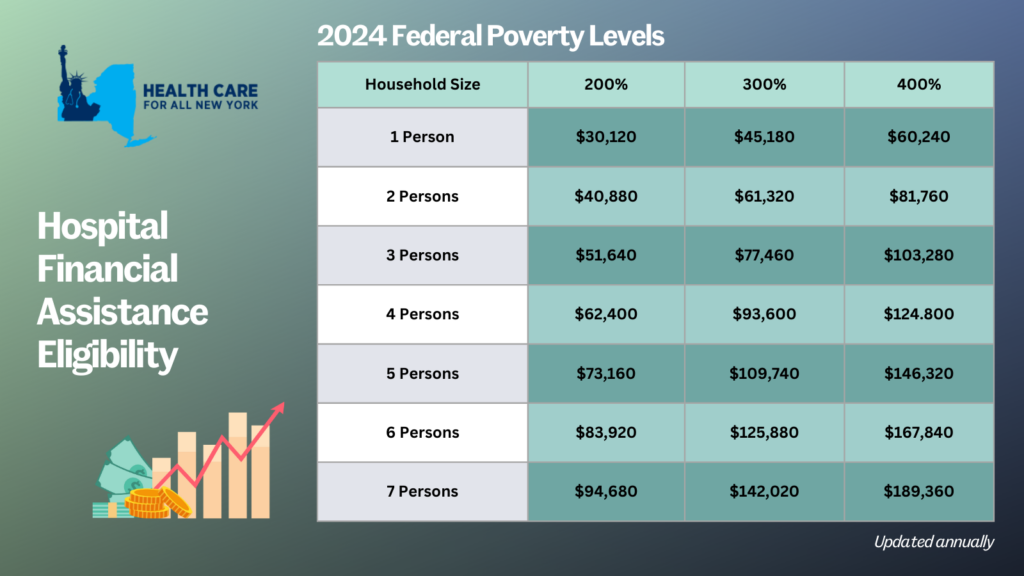
- Patient eligibility for financial assistance will be expanded for those uninsured and underinsured. Under the new law, being underinsured is defined as patients whose paid medical expenses, excluding insurance premiums, exceeds 10 percent of their income within the last 12 months. Uninsured patients will now qualify if their household earns up to 400 percent of the federal poverty level (FPL) and will receive free or discounted care based on a sliding scale (see the table below for eligibility guidelines based on household size and the payment sliding scale). These guidelines will be solely based on the FPL and are updated through the Poverty Guidelines | ASPE.
- Individuals can now apply for hospital financial assistance at any time.
- Hospitals may not sell patients’ debt to third party entities like debt collection agencies. Often these agencies use aggressive and threatening practices to make patients pay medical debt.
- Hospitals are prohibited from bringing lawsuits against patients earning up to 400 percent FPL to collect unpaid medical bills. And lawsuits to collect unpaid balances cannot be brought until 180 days after the first medical bill. Lawsuits have disproportionately affected people of color and low-income residents. For example, according to a 2024 Community Service Society of New York report, over a third of lawsuits filed by State-run hospitals were filed against patients who lived in zip codes where residents are disproportionately people of color. Additionally, nearly all these cases were filed against patients that should have been eligible for hospital financial assistance.
- To measure this impact, hospitals will report to the DOH the number of people that have applied for financial assistance annually including age, gender, race, ethnicity, and insurance status.
With this series of reforms, more New Yorkers will be able to receive affordable hospital care and reduce their chances of incurring medical debt. The HFAL was a landmark reform back in 2006 and has been far improved with these amendments.
Here’s a copy of the form hospitals must use now.
If you need assistance in applying for hospital financial assistance, contact Community Health Advocates at 888-614-5400.

The new 2018 census data numbers are out this this morning.
The bad news is that uninsurance numbers increased across the country by 1.9 million in 2018, despite the positive economy. This was the first increase in uninsured since the Affordable Care Act was fully implemented in 2014. Here’s a New York Times article with more details.
BUT, there’s great news in New York, which was one of just three states in the country to have a decline in our uninsurance numbers, from 1,113,000 in 2017 to 1,041,000 in 2018 (our uninsurance rate declined from 5.7% to 5.4%).
New York’s continued decline in uninsured residents is inextricably linked to its adoption of the high quality, affordable, Essential Plan, which saw an increase in enrollment from 665,000 in 2017 to 739,000 in 2018. Other important factors include:
- One-stop shopping: you can apply for the full spectrum of coverage, including Medicaid, Emergency Medicaid, Child Health Plus, the Essential Plan, Qualified Health Plans and tax credits, all through the same NY State of Health application
- Robust Navigator funding of $27 million a year
Congratulations New Yorkers! And let’s keep up the good work!
 Guest post by Claudia Calhoon, MPH, Director of Health Policy at the New York Immigration Coalition.
Guest post by Claudia Calhoon, MPH, Director of Health Policy at the New York Immigration Coalition.
On Wednesday, December 13, the Assembly Committee on Health, the Assembly Puerto Rican/Hispanic Taskforce, and the Assembly Taskforce on New Americans convened a public hearing on Immigrant access to healthcare. Coverage 4 All, a campaign of Health Care For All New York led by the New York Immigration Coalition and Make the Road New York was instrumental in advocating for the hearing. The campaign’s goal is to expand insurance eligibility to all New Yorkers to reduce disparities in coverage. Barriers to coverage are just one of the many current threats to immigrant health access and quality.
Agencies that provided testimony included the New York State Department of Health, the New York City Mayor’s Office for Immigrants Affairs, New York City Department of Health and Mental Hygiene, and New York City Health + Hospitals. In addition, fifteen individuals from a range of social service, advocacy, health care, and community settings spoke about the impact of the federal administration on immigrant mobility, health utilization, coverage eligibility, and enforcement of language access regulation. Amid a federal landscape hostile to immigrants, New York State programs and protections are increasingly important.
Critical areas of particular attention included making sure that new mothers know they can safely continue to enroll in Medicaid and get prenatal care regardless of their immigration status, and continue to use the Women’s Infants, and Children (WIC) Food and Nutrition services. Another area of common interest among advocates was the opportunity that the state has to expand the Child Health Plus insurance program to cover young adults up to age 29 at a cost of $81 million. Dr. Alan Shapiro, co-founder of Terra Firma, which works with unaccompanied minors, noted that health needs don’t end when young people turn 19. These individuals “still have comprehensive primary care needs. They need access to immunizations, urgent care, sexual and reproductive health services.” The Child Health Plus Expansion is part of Health Care for All New York’s policy agenda, and the key priority of the Coverage 4 All campaign.
Hearing testimony from multiple stakeholders also highlighted the critical nature of improving enforcement of language access regulations, addressing mental health needs of immigrant communities subject to heightened stress under enhanced federal immigration enforcement, and ensuring that safety net hospitals have the revenue they need to care for all New York State residents.
 New York State’s official health plan Marketplace, the NY State of Health (NYSOH), announced this morning that more than 45,000 New Yorkers enrolled in Qualified Health Plan and Essential Plan coverage for the first time during the first four week of Open Enrollment. This represents an 13 percent increase in Marketplace participation compared to the first four weeks of last year’s open enrollment, and there are still two months left to enroll.
New York State’s official health plan Marketplace, the NY State of Health (NYSOH), announced this morning that more than 45,000 New Yorkers enrolled in Qualified Health Plan and Essential Plan coverage for the first time during the first four week of Open Enrollment. This represents an 13 percent increase in Marketplace participation compared to the first four weeks of last year’s open enrollment, and there are still two months left to enroll.
According to the press release, New York’s uninsured rate has reached a new historic low of 4.7 percent compared to 10 percent in 2013.
The release also notes the incredible success of New York’s Basic Health Plan, branded the Essential Plan, which now has nearly 700,000 individuals enrolled.
Open enrollment continues through January 31, 2018. You can enroll in health coverage through the NYSOH website. If you need help enrolling, Navigators are available to provide in-person assistance. Please call (888) 614-5400 to find a Navigator in your area.

