🚨 Take Action to End Medical Debt in NY 🚨
The NY Senate just passed the Fair Medical Debt Reporting Act (S4907A/A6275A), an important step toward protecting patients from the long-term consequences of medical debt.
This bill would prohibit medical debt from being collected by a consumer reporting agency or included in a consumer report. Now we need your help urging the NY Assembly to follow the Senate’s lead and pass the Fair Medical Debt Reporting Act (S4907A/A6275A).
One patient who shared his story with us, David S., had his credit score slashed in half due to medical debt. This means he can no longer buy trucks for his towing business, his main source of income.
David’s story is only one of many. We can’t allow this to keep happening — New Yorkers deserve better. Please take action with us today to protect patients!
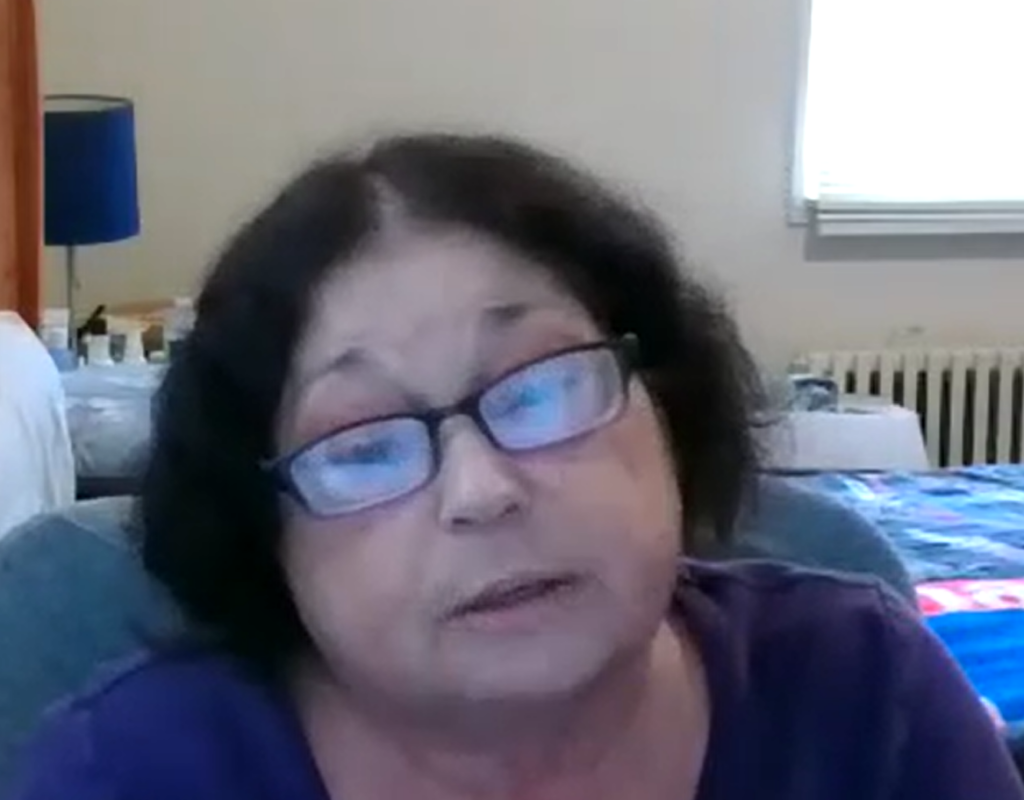
Nancy Rodriguez, a 66-year-old Queens resident, struggles with a number of life-altering cardiopulmonary medical conditions. She works at a doctor’s office despite her disability, to supplement her modest Social Security benefits.
Nancy’s total income is about $30,000 a year, including Social Security — too much to qualify for ordinary Medicaid. Since 2017, she has used the Medicaid Buy-in Program for New Yorkers with Disabilities (MBI-WPD) to cover her medications, multiple specialist visits, and hospitalizations.
Still, Nancy has spent years mired in medical debt. In 2020, her medical bills totaled $500,000, including a 13-day hospitalization for COVID. In 2022 she owed $300,000 for a couple of hospitalizations and a surgery.
“For me to be without health insurance is not acceptable, not even for five minutes.”
Under current law, the MBI-WPD program is limited by income, assets, and age. In her FY2024 Executive Budget, Governor Hochul has proposed expanding the program, so that more New Yorkers with disabilities can work and still qualify for Medicaid coverage.
The Governor has proposed removing the age limit of 65, which Nancy says, “would be a godsend for me.” She does have Medicare, but she does not know how she would manage a Medicare Part B premium, a supplemental “Medigap,” and a drug plan which she figures could amount to $300 per month. “I don’t have that kind of money and I work as many hours as I can. It’s very frightening. I lose a lot of sleep over this.“
We look forward to the passage of New York State’s budget including the expansion of Medicaid Buy-in coverage so that people like Nancy will not have to lose sleep over medical bills and can continue to work. Nancy says, “I am very fortunate that I am able to work and I will continue to work as long as I can do it.”
Let’s keep Nancy working and with critical health coverage.
Today, an extraordinarily diverse group of 61 organizations representing patients, religious leaders, labor organizations, people who are older, have disabilities, immigrants and people of color and more sent a letter to Majority-Leader Andrea Stewart-Cousins and Speaker Carl Heastie calling on elected officials to include the Ounce of Prevention Act (S1366 (2023) | A8441A (2022)) in the final State budget. The bill would reform the state’s Hospital Financial Assistance Law, enabling much-needed support to low-income families burdened by medical debt.
The letter is part of a united effort to end medical debt in New York state. You can show your support through our Phone2Action tool here.
Six percent of New Yorkers have been put into collections over medical bills, with numbers much higher for people of color in parts of the state. Nonprofit hospitals have sued more than 54,000 patients over medical debt they are unable to pay.
Many hospitals fail to offer meaningful financial assistance to their patients, despite receiving $1.1 billion dollars annually in state and federal funding to provide uncompensated care. Still others secure these funds despite failing the New York State Department of Health’s annual audits of their financial aid policies.
The Ounce of Prevention Act would add crucial patient protections to the existing Hospital Financial Assistance Law and increase the number of patients eligible to receive discounted care.
A copy of the letter can be found here.

Two new laws will protect New Yorkers from medical debt in 2023. The first bill, signed by Governor Hochul in November, stops all medical providers from garnishing patients’ wages or placing liens on their homes to collect medical debt judgments (S.6522A/A.7363A). The second bill, signed last week, reforms the practice of imposing facility fees by requiring hospitals and their affiliated providers to notify patients in advance if they charge facility fees and bans the fees for preventive care (S.2521C/A.3470C).
Property liens and wage garnishments were two of the worst consequences for patients sued by their hospitals or doctors after they could not afford medical care. The Community Service Society found that in just two years, New York’s hospitals placed 4,880 liens on patients’ homes. A study of just five hospitals revealed over 1,600 cases where patients’ wages were garnished. Both actions are especially troubling because the data on hospital lawsuits in New York suggests that many patients with medical debt were not adequately screened for financial assistance according to New York State law and IRS regulations (these apply to all hospitals in New York, which does not allow for-profit hospitals). Further, medical debt and all its consequences disproportionately effects people of color. The new law prevents ALL hospitals and other medical providers from taking these extreme actions against their patients—even veterinarians!
Notifying patients about facility fees, and banning them for preventive care, will make medical billing fairer. Facility fees are hospital overhead charges. The Affordable Care Act says that no one may be billed for preventive services, but facility fees still sometimes appear on patients’ bills because they are tied to the location of care, not the service. This law is the first in the nation that prevents facility fees for preventive care. The law also requires providers to notify patients ahead of time about the fee. This gives patients a chance to go somewhere else where they won’t be charged hospital fees for essentially outpatient care. Providers already know your bill will include these fees before you walk in the door—it’s only fair that you do too! (You can hear more from patients about facility fees here and here).
FAQs: What Do Brand New #EndMedicalDebt Protections Mean for NY’ers?
- When do these changes take effect?
Both laws go into effect immediately.
- Does either law apply retroactively?
Both laws are only prospective, not retroactive.
- Can private doctors still place a lien on my home or garnish my wages?
No! The new law applies to money judgments arising from debt collection actions by either hospitals or health care professionals.
- Does the new law apply to all facility fees?
Yes! The new law requires ALL health facilities to disclose when a facility fee is added, and bars these fees for all preventative services—such as a screening mammogram.
- What’s next for the #EndMedicalDebt campaign?
Next, we’re fighting to prevent medical debt before it starts. The Ounce of Prevention Act would require all hospitals in the state to adopt a uniform financial assistance application and policy to simplify the process for patients to apply and be eligible for financial assistance. It would also condition distribution of state Indigent Care Pool (ICP) funds to the hospital’s implementation and compliance with the policy.