The New York Department of Financial Services (the Department) reduced the requested rates by insurance carriers for the individual market by 48 percent for 2026. Carriers initially requested a 13 percent average rate surge, but through New York’s prior approval process, the Department trimmed this figure down to an average of seven percent. Without this process, rates requested by insurance carriers would require New Yorkers to pay an average of $1,291 more annually, or $108 per month, in premiums next year. With the newly approved rates from the Department, the annual increase in premiums is now $678, or $57 per month, for next year.
The table below compares health plans’ initial rate requests with rates that were ultimately approved, providing insight into how this process impacts your health care costs (you can also review our detailed comments on each carrier’s rate request here).
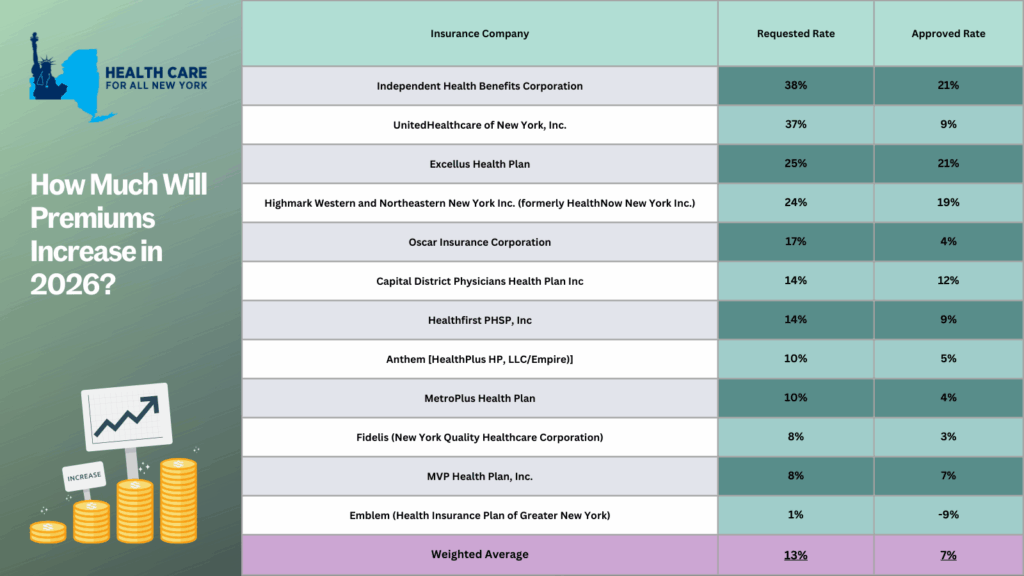
The prior approval process serves as an essential safeguard to curb rising health care costs. For the past two years, the State has approved, on average, steep premium increases of 13% in 2025 and 12% in 2024. With a record number of public comments submitted by consumers, the State reduced the high premium increases requested by individual market insurance carriers. Despite these efforts, any rise in premiums for New Yorkers makes health care even less affordable for consumers, especially with current federal proposals that threaten New York’s health care system:
- Enhanced premium tax credits are set to expire at the end of this year. Unless Congress decides to extend these credits, New Yorkers—who previously received them—can expect a monthly average premium increase of $114.
- New Centers for Medicare and Medicaid Services guidance, set to take effect in 2027, will take away health coverage from 750,000 New York children, from ages 0 to 6, on Medicaid or Child Health Plus.
- The so-called “One Big, Beautiful Bill” is estimated to leave around 1.5 million New Yorkers without health coverage. Learn more about how federal threats impact the State here.
New York should consider additional strategies to protect consumers from steep premium increases beyond the rate review process. HCFANY recommends the State to implement many proposals in HCFANY’s 2025 Policy Agenda that will help patients get affordable care and coverage, like the Primary Care Investment Act, Zero-copay Inhalers, the Fair Pricing Act, or setting up an independent Office of Health Care Affordability.
Many New Yorkers, who purchase their own health coverage through the New York State of Health marketplace, are eligible for subsidies. If you need help switching plans or finding affordable health insurance, the Navigators program offers free, unbiased guidance and can help you understand your premium assistance and coverage options. You can contact Navigators through the CSS Navigator Network at 888-614-5400 or email enroll@cssny.org.
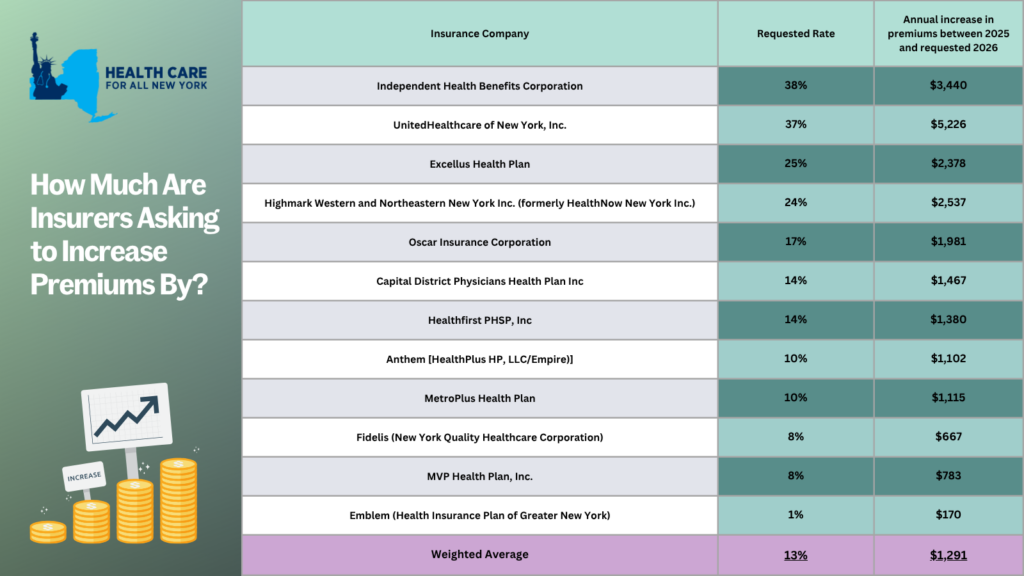
New York’s individual market premiums might increase by up to 13 percent in 2026, forcing consumers to pay an extra $1,291 more annually. New York’s twelve individual market carriers are requesting increases ranging from one percent by Emblem to a staggering 38 percent by Independent Health. These requests far surpass requests from carriers in other states.
In our comments, HCFANY breaks down why DFS should curb each carrier’s specific rate requests to protect patients from another unaffordable increase in health care costs. Find your carrier in the list below:
- Anthem
- CDPHP
- Emblem
- Excellus
- Fidelis
- Healthfirst
- Highmark
- Independent Health
- MetroPlus
- MVP
- Oscar
- United
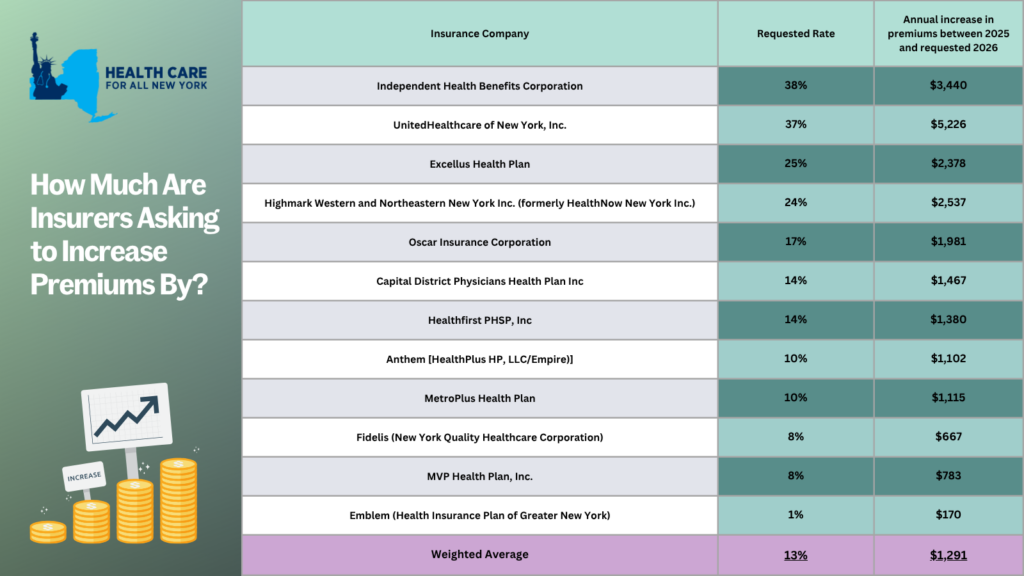
New York’s individual market insurance carriers have asked the Department of Financial Services to allow them to increase premiums by an average of 13% in 2026. This increase would force New Yorkers to pay an average of $1,291 more annually, or $108 monthly, in premiums.
For the next 30 days, starting June 2nd, consumers can make their voices heard by weighing in on the prior approval process.
For the past two years, the State has approved a steep premium increase of 13% in 2025 and 12% in 2024. Another 13% would make health care access even more difficult to reach for many New Yorkers. This percentage increase is greater than wage growth in New York in 2024, as wages have only grown from .4% to 4.6% across the State, depending on the county.
Based on your carrier, premiums could increase between 1% and 38% in 2026, inhibiting New Yorkers’ ability to spend on other essentials like groceries, transportation, or housing. It is critical that the State hears from consumers to ensure that health insurance companies are not making health care even more unaffordable.
Make your voice heard: submit a public comment before July 1, 2025, sharing how steep premium increases would impact your budget or loved ones.
Tell the State how more expensive premiums would impact you by leaving a public comment here by Tuesday, July 1. Share a statement or story on your health care needs and affordability concerns you have, or use the following sample for guidance:
“My plan, (insert carrier name), has asked for a (insert from table below) % premium increase. This would increase my annual premiums by (insert from table below). I already struggle to afford health insurance, and that increase would require me to sacrifice ____.”
New Yorkers anticipating health insurance premiums in the individual market will face
disappointing developments in 2025. The latest data shows that individual market rates
are expected to increase by an average of 13 percent next year. Insurance carriers initially
requested a 17 percent average rate surge for 2025, but through New York’s prior approval
process, the Department of Financial Services has marginally trimmed this figure down. The table below compares health plans’ initial rate requests with rates that were ultimately approved, providing insight into how this process impacts your healthcare costs (you can also review our detailed comments on each carrier’s rate request).
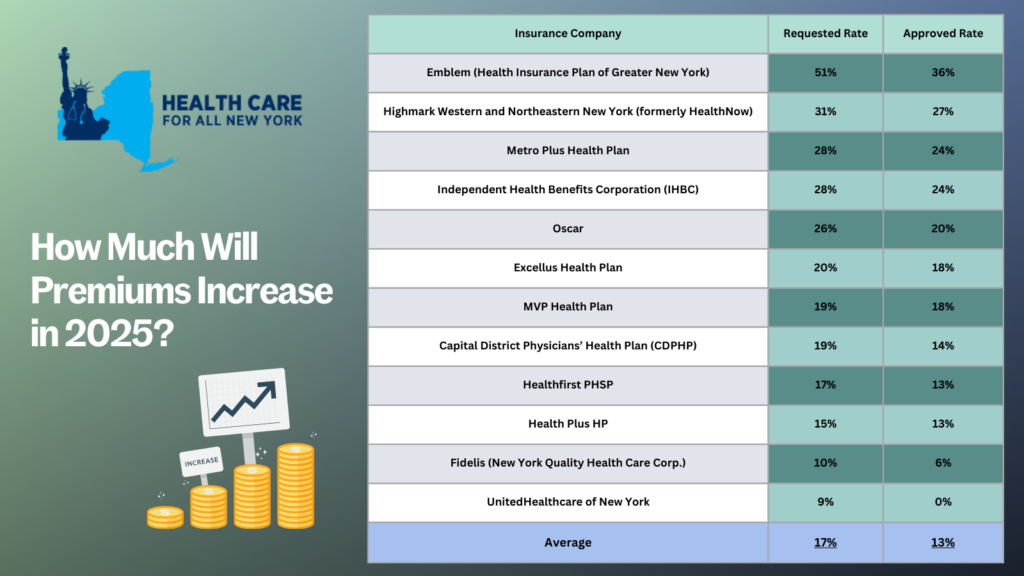
The prior approval process acts as an important safeguard; and while expanded advanced premium tax credits—enacted through the American Rescue Plan during the COVID-19 pandemic—have helped make health insurance more affordable, these tax credits are set to expire in 2025. This 13 percent increase will be a financial burden for many New Yorkers. New York should consider additional strategies to protect consumers from steep premium increases beyond the rate review process. States—such as Connecticut, Delaware, Massachusetts, Nevada, New Jersey, Oregon, Rhode Island, and Washington—have already taken steps in this direction, setting up Health Care Cost Containment task forces or agencies.
If you’re concerned about health insurance costs, there’s good news. Most New Yorkers
purchasing their own health coverage are eligible for subsidies that can help. To explore
your options and learn more about available subsidies, visit the NY State of Health
enrollment site. If you need help switching plans or finding affordable health insurance, the
Navigators program offers free, unbiased guidance and can help you understand your
premium assistance and coverage options. You can contact Navigators through the CSS
Navigator Network at 888-614-5400 or email enroll@cssny.org. Additionally, you can reach out to NY State of Health assistors online or by calling 855-355-5777.
