The New York Department of Financial Services (the Department) reduced the requested rates by insurance carriers for the individual market by 48 percent for 2026. Carriers initially requested a 13 percent average rate surge, but through New York’s prior approval process, the Department trimmed this figure down to an average of seven percent. Without this process, rates requested by insurance carriers would require New Yorkers to pay an average of $1,291 more annually, or $108 per month, in premiums next year. With the newly approved rates from the Department, the annual increase in premiums is now $678, or $57 per month, for next year.
The table below compares health plans’ initial rate requests with rates that were ultimately approved, providing insight into how this process impacts your health care costs (you can also review our detailed comments on each carrier’s rate request here).
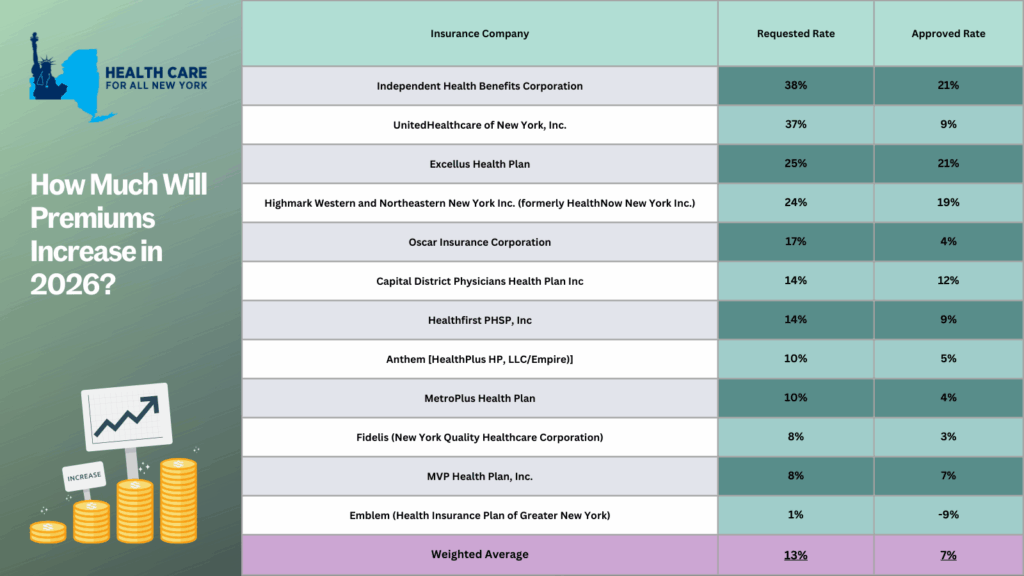
The prior approval process serves as an essential safeguard to curb rising health care costs. For the past two years, the State has approved, on average, steep premium increases of 13% in 2025 and 12% in 2024. With a record number of public comments submitted by consumers, the State reduced the high premium increases requested by individual market insurance carriers. Despite these efforts, any rise in premiums for New Yorkers makes health care even less affordable for consumers, especially with current federal proposals that threaten New York’s health care system:
- Enhanced premium tax credits are set to expire at the end of this year. Unless Congress decides to extend these credits, New Yorkers—who previously received them—can expect a monthly average premium increase of $114.
- New Centers for Medicare and Medicaid Services guidance, set to take effect in 2027, will take away health coverage from 750,000 New York children, from ages 0 to 6, on Medicaid or Child Health Plus.
- The so-called “One Big, Beautiful Bill” is estimated to leave around 1.5 million New Yorkers without health coverage. Learn more about how federal threats impact the State here.
New York should consider additional strategies to protect consumers from steep premium increases beyond the rate review process. HCFANY recommends the State to implement many proposals in HCFANY’s 2025 Policy Agenda that will help patients get affordable care and coverage, like the Primary Care Investment Act, Zero-copay Inhalers, the Fair Pricing Act, or setting up an independent Office of Health Care Affordability.
Many New Yorkers, who purchase their own health coverage through the New York State of Health marketplace, are eligible for subsidies. If you need help switching plans or finding affordable health insurance, the Navigators program offers free, unbiased guidance and can help you understand your premium assistance and coverage options. You can contact Navigators through the CSS Navigator Network at 888-614-5400 or email enroll@cssny.org.
With the recent release of the Senate and Assembly One-House budgets, HCFANY is excited to see some of our policy agenda items included. However, HCFANY is also disappointed that key proposals to protect and improve health care coverage for many New Yorkers were left out. Read below for HCFANY’s response to the One-House budgets:
HCFANY supports the following proposals in either the Assembly or the Senate One-House Budget or both:
- Strengthen maternal and reproductive health care access.
- Cover more lactation support services under Medicaid, including allowing certified lactation consultants to enroll as Medicaid providers and covering breast pump supplies.
Primary Care spending: In the United States, less than five cents of every dollar we spend on health care goes to primary care doctors and nurses, even though they handle a third of health care visits. In New York, nearly 70 percent of all emergency room visits are non-emergent and could be better treated in a primary care setting, over double the national rate. HCFANY strongly supports the inclusion of the provisions of the Primary Care Investment Act in the Senate’s One-House Budget, which requires insurance carriers to increase spending on primary care by one percent each year until they reach a target of 12.5 percent. Investment in primary care can reduce the prevalence of chronic diseases and overall health care spending. According to a recently released survey on health care affordability, 79 percent of New Yorkers support requiring insurance carriers to gradually increase spending on primary care. Many other states have also enacted similar policies requiring increased primary care spending (e.g., Colorado, Delaware, Oregon, and Rhode Island). New York should follow suit.
Maternal, reproductive, and lactation care: In New York, Black mothers are five times more likely to have a pregnancy-related death than their White counterparts. HCFANY strongly supports initiatives that tackle racial inequities within New York’s health care system and is excited to see greater and continued support from New York’s Legislature for maternal and reproductive health care. Almost half of births in New York are covered under Medicaid, and with current federal threats that may cut funding for Medicaid—providing health care access to around 7 million New Yorkers. New York can use the budget to safeguard access to care for many New York mothers.
HCFANY supports the following initiatives introduced in the Executive Budget but urges the Legislature and the Governor to adopt slight modifications in the final budget:
- Strengthen the New York Department of Health’s (DOH) oversight of material health care transactions and require public disclosure and allow public participation during the health care transaction process. A material health care transaction includes mergers, acquisitions, or a form of partnership with the purpose of administering contracts with health plans, third-party administrators, pharmacy benefit managers, or health care providers. What is excluded from this definition is partnerships for clinical trials or transactions that result in a health care entity increasing its total gross in-state revenue by less than $25 million.
HCFANY supports granting the DOH authority to determine a health care transaction’s potential market and cost impact and the post-closure impact on costs, quality, access, health equity, and competition. Additionally, the Executive budget proposes that transactions require written notice before the transaction closes to include whether either a party or parent company owns a health care entity that has closed, is in the process of closing, or has reduced its services provided. In the Senate’s One-House budget, HCFANY supports the addition of extending the notification time frame for closures from 60 to 90 days.
HCFANY, separately, urges the Legislature to make amendments to the language to improve transparency and consumer engagement for this process by (1) requiring full public disclosure of the material transactions, (2) extending the time to file such a transaction, and (3) allowing the public to provide input on the proposed transactions to the DOH, similar to the provisions of the Local Input for Community Healthcare Act (LICH) (S1226/A6004) passed by both houses of the Legislature and vetoed by the Governor last year. The LICH bill would require the approval of closures of a hospital or maternity, emergency, or mental health services to consider findings from a Health Equity Impact Assessment, and closures must be reviewed in public sessions by the State’s Public Health and Health Planning Council.
HCFANY is disappointed that the following initiatives are not included in the One-House Budgets:
- Include the No Blank Checks Act (S6375), which would create a uniform patient financial liability form that includes a good faith estimate of what a patient owes financially for the care or service they will receive.
- Include the Fair Pricing Act (S705/A2140), which would limit prices on routine medical services to 150% of the Medicare rate.
- Redistribute some of the $1.4 billion from Managed Care Organization (MCO) tax revenue for direct patient support and a rainy-day fund.
No Blank Checks: When patients walk into an appointment for a health care service, they are often required to sign a form agreeing to pay for any charges not covered by my insurance before they receive any care. This form legally binds them to pay for the service they get without knowing the outcome, how much will be covered by insurance, or whether their provider will bill correctly. It is essentially a blank check. The provisions of the No Blank Checks Act would create a uniform patient financial liability form that includes a good faith estimate of a patient’s financial obligation for their care. If patients are liable to pay for the service beforehand, health care services should inform them of how much it will cost. New Yorkers need greater price transparency, and many agree, as 92 percent of New Yorkers endorse requiring hospitals and doctors to provide up-front cost estimates to consumers.
Fair Pricing: According to 32BJ Health Fund claims data, the exact same service can cost $1,000 more at a hospital-owned outpatient department compared to a doctor’s office. Spending on hospital care is the biggest contributor to rising health care spending in New York, rising twice as fast as income and four times as fast as inflation. Rising prices directly affect New Yorkers as around two-thirds of them have experienced a health care affordability burden this year, with even more worried about affording care in the future. The Fair Pricing Act, which caps prices for routine services at a reasonable 150% of Medicare rates, would save the State an estimated $1.1 billion, $213 million of which would be saved annually by New Yorkers in reduced out-of-pocket costs. It is also supported by 86% of New Yorkers.
MCO tax: The MCO tax allows the State to draw down federal funds by taxing Medicaid and the Essential Plan MCOs to receive a federal match. The State then reimburses MCOs to make them whole and pockets the additional revenue. The Executive budget is allocating a significant portion of this revenue to hospitals. However, HCFANY urges the Governor and the Legislature to come together to reallocate some of these funds to support patients directly in the final budget. With federal threats to cut funding to Medicaid and Affordable Care Act health programs, the State can use this tax revenue to protect New Yorkers’ access to health care coverage by allocating some of this revenue to principal reserves or rainy-day funds. Medicaid provides health and financial security for seniors, children, and working-class families, and it is a critical source of funding for hospitals, clinics, community health centers, and long-term care facilities. The State should use the MCO tax revenue as an opportunity to prepare for potential cuts to federal health programs, including Medicaid.
- Worried about federal threats to health coverage? Call key New York Members of Congress today and ask them to stop federal threats to health care in order to pay for tax breaks for millionaires. They need to hear from New Yorkers on why they need to vote to protect our access to health care: click here.
- Learn how federal threats affect New York State and each of its congressional districts: click here.
Stay tuned for our comments on the final State budget releases.
Every September, healthcare providers see a rise in asthma-related hospitalizations. The third week of September is known as Asthma Peak Week; ragweed levels—a common fall pollen allergy—are peaking, mold counts are increasing as leaves start to fall, children are catching respiratory infections as they go back to school, and flu season is just beginning. Proper asthma control is essential to stay healthy and manage symptoms during this month. However, for many, healthcare costs are making it difficult to manage or control their symptoms.
In New York, asthma impacts more than 1.4 million adults and an estimated 315,000 children, according to the New York State Department of Health and the US Center for Disease Control, respectively as of 2021. The price of asthma inhalers, a lifesaving and sustaining device, has drastically increased over the past decade and can cost an individual up to $645 a month, according to the Senate Committee on Health, Education, Labor and Pensions (HELP). At these high prices, some patients are rationing doses or even abandoning their inhalers—which can lead to unnecessary hospitalizations and even preventable deaths. Though with insurance, patients share the cost of an inhaler with their insurance provider through a deductible or copayment—even those with health coverage struggle to afford inhalers.
Asthma rates and asthma-related complications disproportionately affect communities of color and low-income communities in New York. Black New Yorkers are over nine times more likely to visit the Emergency Department (ED) for asthma-related complications than their White counterparts—four times more likely for Hispanic New Yorkers. Asthma-related ED visits are also three times as frequent for individuals in low-income zip codes when compared to those in higher-income zip codes. Asthma is an apparent public health issue affecting those already facing economic and environmental disparities.
Earlier this year, with pressure from the HELP committee and Senator Bernie Sanders, three of the largest producers of inhalers—AstraZeneca, Boehringer Ingelheim, and GlaxoSmithKline—agreed to cap their inhaler products, for both asthma and chronic obstructive pulmonary disease, at $35 or less per month. This price cap will be available for those on commercial insurance and those uninsured, which will be automatically applied at local pharmacies or accessed with a copay card. However, those enrolled in government insurance programs, like Medicare or Medicaid, are left behind due to federal restrictions.
Luckily, New York legislators, Assembly Member Jessica González-Rojas and State Senator Gustavo Rivera, have proposed a bill to remove this financial barrier by eliminating deductibles, copayments, coinsurance, or other cost-sharing requirements for inhalers and require insurance coverage for inhalers at no cost. González-Rojas introduced this legislation because of its significance to her district, representing communities in Queens, that have high rates of hospitalization due to asthma. Rivera represents the northwest Bronx, a borough with substantially higher asthma mortality rates than other New York City boroughs. We commend both González-Rojas and Rivera for taking these necessary actions in trying to address New York’s asthma crisis.
Minnesota and Illinois, Washington, and New Jersey have passed similar legislation that caps the cost-sharing requirements of inhalers at $25, $35, and $50 per month, respectively. We need New York to step up to the plate to save lives and treat asthma. “This smart bill will ensure that insurance cost-sharing is never a barrier to accessing life-sustaining inhalers for those who need it,” said Elisabeth R. Benjamin, Vice President of Health Initiatives at the Community Service Society of New York.
Ellen, a Long Islander, received an unexpected and unwelcomed bill from a hospital system when she went to her doctor’s office for a biopsy. She was not anticipating a “net facility charge” of $2,142 which she was not informed of. She protests that she was not provided with any notice that she would be charged extra for a facility charge when she was visiting a doctor. She also received a bill for net charges of $618.07 from the Doctor. “Had I known that was the billing practice, I would not have visited this doctor,” she says.
She adds, “There was nothing from the doctor or her staff, or from the circumstances of the procedure, that would have indicated to me that I was being treated at a hospital. Both the examination and the procedure took place in a typical examining room at the doctor’s office. I was not even placed on a special chair for the procedure— I was wearing my street clothes.” The facility fee is not a charge for an actual health service. As of now, it is a legal way for the hospital that bought your doctor’s office or clinic to add the hospital’s overhead cost to your doctor’s bill. Health Insurance often will not pay these facility fees, leaving the patient stuck with the bill, uninsured patients are always stuck with these facility fee bills.
A new bill, the (A3470B/S2521B), would regulate these health care facility fees and provide some semblance of protection by not allowing a provider to seek payment of these fees if not covered by insurance, unless they had notified and explained the fee and amount at least seven days in advance of the procedure. If approved by the New York State Legislature and signed into law by the Governor, the would ensure that patients will no longer be held responsible for this kind of surprise bill and what happened to Ellen will no longer happen to any other New Yorker. The bill would also prevent facility fees for preventive care – New York will be the first state to do so if it passes!
