The season of giving is coming early for many New Yorkers seeking hospital care this year. As of last month, amendments to New York’s Hospital Financial Assistance Law (HFAL) will make it easier to apply for and cover more patients under financial assistance programs. The HFAL, also known as Manny’s Law, was implemented in 2006 in response to the death of Manny Lanza, 24. Lanza passed away after being denied life-saving surgery due to his uninsured status.
Financial assistance programs help many patients receive affordable care on a sliding fee scale based solely on their household income. This includes patients who are uninsured or those with insurance, but medical costs are a big strain on their income. Rising hospital prices in recent years have left many patients unable to afford the care they need, often leading them to incur medical debt. A 2023 Urban Institute reported that 740,000 New Yorkers had medical debt, with nearly half of them owing $500 or more. This updated HFAL will streamline the process and expand the eligibility of hospital financial assistance. New Yorkers will finally be able to have some more relief from medical debt and rising healthcare costs.
The following changes will be made to HFAL and medical debt in New York.
- All hospitals licensed by the New York State Department of Health (NYSDOH) are required to use a Uniform Hospital Financial Assistance form and inform patients of financial assistance availability in writing during registration and at discharge (regardless of the hospital’s participation in the Indigent Care Pool). Eligibility will not consider the patient’s immigration status. Before this amendment, many patients were never informed financial assistance existed and many hospitals requested information that was not legally required, like Social Security Numbers or tax returns, which often scared patients away from applying.
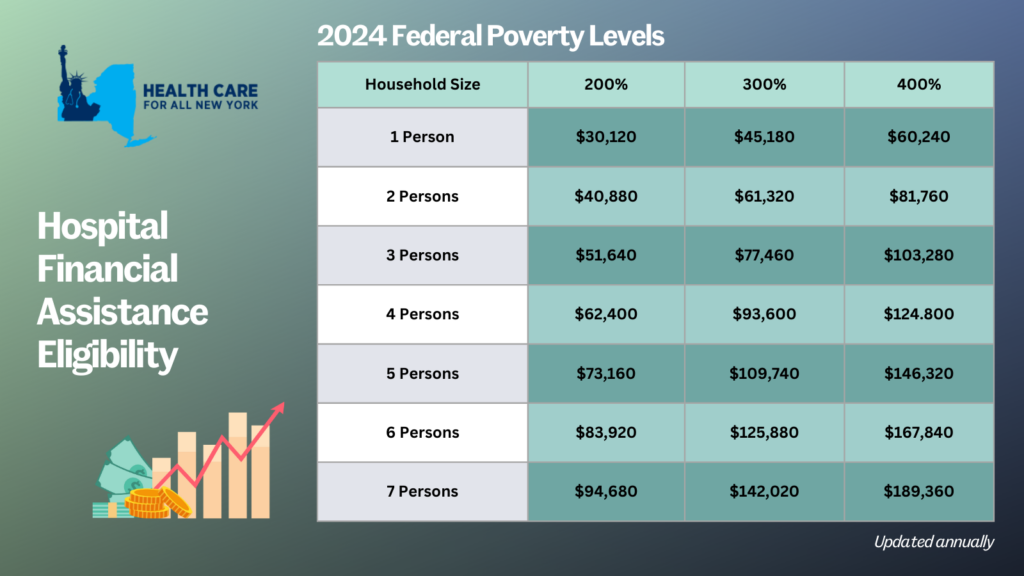
- Patient eligibility for financial assistance will be expanded for those uninsured and underinsured. Under the new law, being underinsured is defined as patients whose paid medical expenses, excluding insurance premiums, exceeds 10 percent of their income within the last 12 months. Uninsured patients will now qualify if their household earns up to 400 percent of the federal poverty level (FPL) and will receive free or discounted care based on a sliding scale (see the table below for eligibility guidelines based on household size and the payment sliding scale). These guidelines will be solely based on the FPL and are updated through the Poverty Guidelines | ASPE.
- Individuals can now apply for hospital financial assistance at any time.
- Hospitals may not sell patients’ debt to third party entities like debt collection agencies. Often these agencies use aggressive and threatening practices to make patients pay medical debt.
- Hospitals are prohibited from bringing lawsuits against patients earning up to 400 percent FPL to collect unpaid medical bills. And lawsuits to collect unpaid balances cannot be brought until 180 days after the first medical bill. Lawsuits have disproportionately affected people of color and low-income residents. For example, according to a 2024 Community Service Society of New York report, over a third of lawsuits filed by State-run hospitals were filed against patients who lived in zip codes where residents are disproportionately people of color. Additionally, nearly all these cases were filed against patients that should have been eligible for hospital financial assistance.
- To measure this impact, hospitals will report to the DOH the number of people that have applied for financial assistance annually including age, gender, race, ethnicity, and insurance status.
With this series of reforms, more New Yorkers will be able to receive affordable hospital care and reduce their chances of incurring medical debt. The HFAL was a landmark reform back in 2006 and has been far improved with these amendments.
Here’s a copy of the form hospitals must use now.
If you need assistance in applying for hospital financial assistance, contact Community Health Advocates at 888-614-5400.
Every September, healthcare providers see a rise in asthma-related hospitalizations. The third week of September is known as Asthma Peak Week; ragweed levels—a common fall pollen allergy—are peaking, mold counts are increasing as leaves start to fall, children are catching respiratory infections as they go back to school, and flu season is just beginning. Proper asthma control is essential to stay healthy and manage symptoms during this month. However, for many, healthcare costs are making it difficult to manage or control their symptoms.
In New York, asthma impacts more than 1.4 million adults and an estimated 315,000 children, according to the New York State Department of Health and the US Center for Disease Control, respectively as of 2021. The price of asthma inhalers, a lifesaving and sustaining device, has drastically increased over the past decade and can cost an individual up to $645 a month, according to the Senate Committee on Health, Education, Labor and Pensions (HELP). At these high prices, some patients are rationing doses or even abandoning their inhalers—which can lead to unnecessary hospitalizations and even preventable deaths. Though with insurance, patients share the cost of an inhaler with their insurance provider through a deductible or copayment—even those with health coverage struggle to afford inhalers.
Asthma rates and asthma-related complications disproportionately affect communities of color and low-income communities in New York. Black New Yorkers are over nine times more likely to visit the Emergency Department (ED) for asthma-related complications than their White counterparts—four times more likely for Hispanic New Yorkers. Asthma-related ED visits are also three times as frequent for individuals in low-income zip codes when compared to those in higher-income zip codes. Asthma is an apparent public health issue affecting those already facing economic and environmental disparities.
Earlier this year, with pressure from the HELP committee and Senator Bernie Sanders, three of the largest producers of inhalers—AstraZeneca, Boehringer Ingelheim, and GlaxoSmithKline—agreed to cap their inhaler products, for both asthma and chronic obstructive pulmonary disease, at $35 or less per month. This price cap will be available for those on commercial insurance and those uninsured, which will be automatically applied at local pharmacies or accessed with a copay card. However, those enrolled in government insurance programs, like Medicare or Medicaid, are left behind due to federal restrictions.
Luckily, New York legislators, Assembly Member Jessica González-Rojas and State Senator Gustavo Rivera, have proposed a bill to remove this financial barrier by eliminating deductibles, copayments, coinsurance, or other cost-sharing requirements for inhalers and require insurance coverage for inhalers at no cost. González-Rojas introduced this legislation because of its significance to her district, representing communities in Queens, that have high rates of hospitalization due to asthma. Rivera represents the northwest Bronx, a borough with substantially higher asthma mortality rates than other New York City boroughs. We commend both González-Rojas and Rivera for taking these necessary actions in trying to address New York’s asthma crisis.
Minnesota and Illinois, Washington, and New Jersey have passed similar legislation that caps the cost-sharing requirements of inhalers at $25, $35, and $50 per month, respectively. We need New York to step up to the plate to save lives and treat asthma. “This smart bill will ensure that insurance cost-sharing is never a barrier to accessing life-sustaining inhalers for those who need it,” said Elisabeth R. Benjamin, Vice President of Health Initiatives at the Community Service Society of New York.
Learn what’s in the HEROES Act from New York’s Congressional leaders and advocates, and find out what you can do get it enacted! The HEROES Act, which already passed the House, would provide much needed pandemic relief and protect the programs, like Medicaid, that are helping people get by during the crisis. Read more here, and register for the virtual rally here.
Action step – Sign-ons needed by close of business tomorrow:
Sign your organization on to this letter (link) drafted by Citizen Action of New York, Medicaid Matters New York, Health Care For America Now, and HCFANY. The letter thanks Senators Schumer and Gillibrand for their work so far to protect New Yorkers during the pandemic – and describes what New Yorkers need included in an enacted version of the HEROES Act. Add your organization’s name here.
Also Coming Up:
100 Years On: Celebrating and Championing Our Civil Rights and Social Programs
So many of our most important civil rights laws and social programs were created in July and August – the National Labor Relations Act (1935), Social Security (1935), the Civil Rights Act (1964), Medicare and Medicaid (1965), the Americans with Disabilities Act (1990). Join fellow New York advocates to celebrate these achievements and fight for justice!
- Dessert Party for Democracy: A Multi-Generational Celebration. We will share pictures and videos of everyday people sharing stories and holding signs saying “I celebrate X because…” We will end with a toast and display of your dessert, holding up signs, including all members of your family or household. August 13, 7:00 – 8:00 PM, register here.
- Renewing the American Promise: Defending and Expanding Our Social Contract. Learn more about the civil rights and social programs that everyday New Yorkers benefit from and learn how these programs and laws are at risk. August 19, 12:00 – 1:00PM, register here.
 Guest post by Lois Uttley and Emma Chessen.
Guest post by Lois Uttley and Emma Chessen.
Remember St. Vincent’s Hospital in Manhattan, now the site of luxury condos? How about Millard Fillmore Gates Hospital, now an assisted living facility? Or Cornwall Hospital, which was gradually dismantled as an inpatient facility and replaced with outpatient care? Perhaps you were a patient of Amsterdam Memorial Hospital, which was closed in 2014 and converted into an ambulatory surgery center. Wonder what’s happening to community hospitals all over New York?
If so, you are not alone. Over the last 20 years, 41 New York hospitals have closed all of their inpatient services, affecting consumers across the state. Many of the remaining hospitals, particularly smaller community hospitals, are joining large health systems. In fact, the 12 largest health care systems now control half of all acute care hospitals in the state and 70 percent of the inpatient acute care beds.
Why is all this hospital consolidation happening? One cause is the movement of medical care into outpatient settings, leaving unneeded hospital beds. Another factor is the rise of complicated reimbursement schemes that require the sophistication of a large hospital system. Some urban hospitals are suffering financially from treating a high percentage of patients who are uninsured or have Medicaid, as opposed to better paying commercial insurance, and receive inadequate government support for serving these patients.
What does consolidation mean for consumers? Hospitals joining systems often argue that quality of care and financial stability will be improved. But, hospital consolidation can have negative consequences for affected consumers. Local hospitals that join large systems are sometimes downsized, closed or transformed into outpatient facilities. Patients needing advanced care may be referred to academic medical centers located an hour or more away. Decision-making often shifts to out-of-town system executives who don’t know the community and the specific health needs of the local population. Consolidation can also cause the price of health care to go up.
With such significant consequences for patients, it’s important that consumers have a say when their local hospitals are proposing mergers or other types of consolidation. But all too often, that doesn’t happen, according to year-long study MergerWatch recently completed with the support of the New York State Health Foundation. Our report, “Empowering New York Consumers in an Era of Hospital Consolidation,” concluded that New York’s 54-year-old Certificate of Need (CON) system of state hospital oversight needs to be updated to ensure that consumers are notified and engaged when their local hospitals propose to join health systems or plan to downsize, close or transform the way they deliver health services.
MergerWatch’s recommendations include requiring public hearings in affected communities prior to hospital closings or elimination of key services, such as maternity care or the emergency department. MergerWatch urges that when health systems are taking over local hospitals, they should be required to disclose whether services might be downsized or transferred elsewhere in the system, and predict whether the transaction might cause the price of health care to go up. The report also recommends changes to the New York State Department of Health website to make it easier for consumers to find information about proposed hospital consolidations and submit comments.
The report urges a stronger voice for consumers in state decision-making through increased consumer representation on the state Public Health and Health Planning Council (PHHPC), which considers the most important hospital transactions. The PPHPC has only one consumer seat, and it has been vacant since 2016, while the majority of council members (including the chair) are employed by hospitals and other health providers. By contrast, in New Jersey and Maryland the majority of hospital review board members are consumers and in Delaware, the chair of the review board must be drawn from the “public at large.”
As hospital consolidation continues around the state, MergerWatch hopes to see an improved and more transparent state review process that informs, engages and carefully considers comments from the consumers whose health care will be dramatically affected. Want to learn more about our findings and recommendations, and get involved in helping improve the system? Join our webinar on July 19 at 2 pm.
Lois Uttley, MPP, lead author of the new report, is founder of MergerWatch and Director of Women’s Health for Community Catalyst. She serves on the steering committee of Health Care for All NY. Emma Chessen, co-author of the report, received her Master’s in Public Health in May from Columbia University’s Mailman School of Public Health.

