The season of giving is coming early for many New Yorkers seeking hospital care this year. As of last month, amendments to New York’s Hospital Financial Assistance Law (HFAL) will make it easier to apply for and cover more patients under financial assistance programs. The HFAL, also known as Manny’s Law, was implemented in 2006 in response to the death of Manny Lanza, 24. Lanza passed away after being denied life-saving surgery due to his uninsured status.
Financial assistance programs help many patients receive affordable care on a sliding fee scale based solely on their household income. This includes patients who are uninsured or those with insurance, but medical costs are a big strain on their income. Rising hospital prices in recent years have left many patients unable to afford the care they need, often leading them to incur medical debt. A 2023 Urban Institute reported that 740,000 New Yorkers had medical debt, with nearly half of them owing $500 or more. This updated HFAL will streamline the process and expand the eligibility of hospital financial assistance. New Yorkers will finally be able to have some more relief from medical debt and rising healthcare costs.
The following changes will be made to HFAL and medical debt in New York.
- All hospitals licensed by the New York State Department of Health (NYSDOH) are required to use a Uniform Hospital Financial Assistance form and inform patients of financial assistance availability in writing during registration and at discharge (regardless of the hospital’s participation in the Indigent Care Pool). Eligibility will not consider the patient’s immigration status. Before this amendment, many patients were never informed financial assistance existed and many hospitals requested information that was not legally required, like Social Security Numbers or tax returns, which often scared patients away from applying.
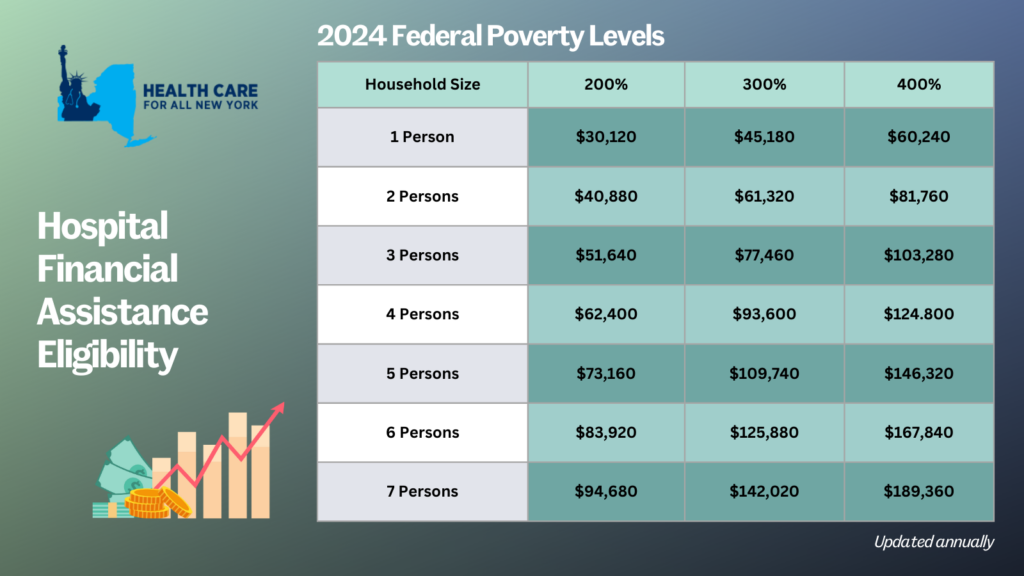
- Patient eligibility for financial assistance will be expanded for those uninsured and underinsured. Under the new law, being underinsured is defined as patients whose paid medical expenses, excluding insurance premiums, exceeds 10 percent of their income within the last 12 months. Uninsured patients will now qualify if their household earns up to 400 percent of the federal poverty level (FPL) and will receive free or discounted care based on a sliding scale (see the table below for eligibility guidelines based on household size and the payment sliding scale). These guidelines will be solely based on the FPL and are updated through the Poverty Guidelines | ASPE.
- Individuals can now apply for hospital financial assistance at any time.
- Hospitals may not sell patients’ debt to third party entities like debt collection agencies. Often these agencies use aggressive and threatening practices to make patients pay medical debt.
- Hospitals are prohibited from bringing lawsuits against patients earning up to 400 percent FPL to collect unpaid medical bills. And lawsuits to collect unpaid balances cannot be brought until 180 days after the first medical bill. Lawsuits have disproportionately affected people of color and low-income residents. For example, according to a 2024 Community Service Society of New York report, over a third of lawsuits filed by State-run hospitals were filed against patients who lived in zip codes where residents are disproportionately people of color. Additionally, nearly all these cases were filed against patients that should have been eligible for hospital financial assistance.
- To measure this impact, hospitals will report to the DOH the number of people that have applied for financial assistance annually including age, gender, race, ethnicity, and insurance status.
With this series of reforms, more New Yorkers will be able to receive affordable hospital care and reduce their chances of incurring medical debt. The HFAL was a landmark reform back in 2006 and has been far improved with these amendments.
Here’s a copy of the form hospitals must use now.
If you need assistance in applying for hospital financial assistance, contact Community Health Advocates at 888-614-5400.
By Bob Cohen, Policy Director, Citizen Action New York
The COVID-19 pandemic is exposing just how broken the US health care system is, including our inability to control disease outbreaks when many people simply cannot afford basic medical care. Patients should never fear seeking medical care because of cost, but for many New Yorkers that is the reality. And a new report by the Community Service Society highlights one of the worst outcomes for patients who cannot pay their medical bills – lawsuits filed against them by the hospitals they turned to for help. The report, “Discharged Into Debt,” finds that New York hospitals have filed over 30,000 debt collection lawsuits in the past five years. The study only looked at hospitals in 26 of New York’s 62 counties – which means the actual number of lawsuits is much higher.
New York State’s non-profit hospitals have a social mission. Legally, they are charities that pay no federal, state or local taxes and receive a total of $1.1 billion each year from the ICP. As a condition for receiving this funding, hospitals are required to offer financial assistance to patients without insurance.
The report, based on an examination of the New York State Ecourts public database and a sample of hundreds of individual case files, documented a number of abusive practices by New York hospitals. For example, hospitals claimed in legal papers that they were entitled to payment for unspecified items like “miscellaneous” and “ancillary procedures” charges. And, because New York allows hospitals to charge an outrageous 9% interest rate on outstanding bills and to tack on court fees on top of that, the median amount the hospital sued on was $1,900 but the median judgment amount was $2,300. In many cases, hospitals sued patients that were eligible for financial assistance without offering it, as required by law.
The report also found large racial disparities in the treatment of patients that owe medical debt, particularly upstate. In counties like Onondaga (Syracuse), Monroe (Rochester), Albany and Erie (Buffalo), a much higher proportion of people were referred to collections for medical debt in communities of color than white communities.
And, the study documents, patients were almost always totally outmatched by large collection law firms retained by the hospitals. Process servers often illegally serve relatives or co-tenants instead of patients, violating basic provisions of the U.S. constitution and in state laws designed to make sure people have reasonable notice of lawsuits so they can adequately defend themselves. And, 97% of the patients in the study were unrepresented and didn’t even attempt to respond to the lawsuit. The result is often wrecked credit, and unpaid judgments that threaten the financial futures of consumers and their families.
The CSS report adds to the case for passage of the Patient Medical Debt Protection Act (A.8639/S.6757), which addresses some of the most egregious medical billing practices. Fixing these practices, including lawsuit abuses, is a critical step in fixing our broken health care system and making health care affordable to low and moderate income New Yorkers.
 Guest post by Claudia Calhoon, MPH, Director of Health Policy at the New York Immigration Coalition.
Guest post by Claudia Calhoon, MPH, Director of Health Policy at the New York Immigration Coalition.
On Wednesday, December 13, the Assembly Committee on Health, the Assembly Puerto Rican/Hispanic Taskforce, and the Assembly Taskforce on New Americans convened a public hearing on Immigrant access to healthcare. Coverage 4 All, a campaign of Health Care For All New York led by the New York Immigration Coalition and Make the Road New York was instrumental in advocating for the hearing. The campaign’s goal is to expand insurance eligibility to all New Yorkers to reduce disparities in coverage. Barriers to coverage are just one of the many current threats to immigrant health access and quality.
Agencies that provided testimony included the New York State Department of Health, the New York City Mayor’s Office for Immigrants Affairs, New York City Department of Health and Mental Hygiene, and New York City Health + Hospitals. In addition, fifteen individuals from a range of social service, advocacy, health care, and community settings spoke about the impact of the federal administration on immigrant mobility, health utilization, coverage eligibility, and enforcement of language access regulation. Amid a federal landscape hostile to immigrants, New York State programs and protections are increasingly important.
Critical areas of particular attention included making sure that new mothers know they can safely continue to enroll in Medicaid and get prenatal care regardless of their immigration status, and continue to use the Women’s Infants, and Children (WIC) Food and Nutrition services. Another area of common interest among advocates was the opportunity that the state has to expand the Child Health Plus insurance program to cover young adults up to age 29 at a cost of $81 million. Dr. Alan Shapiro, co-founder of Terra Firma, which works with unaccompanied minors, noted that health needs don’t end when young people turn 19. These individuals “still have comprehensive primary care needs. They need access to immunizations, urgent care, sexual and reproductive health services.” The Child Health Plus Expansion is part of Health Care for All New York’s policy agenda, and the key priority of the Coverage 4 All campaign.
Hearing testimony from multiple stakeholders also highlighted the critical nature of improving enforcement of language access regulations, addressing mental health needs of immigrant communities subject to heightened stress under enhanced federal immigration enforcement, and ensuring that safety net hospitals have the revenue they need to care for all New York State residents.
 Guest post by Max Hadler, Senior Health Policy Manager at the New York Immigration Coalition.
Guest post by Max Hadler, Senior Health Policy Manager at the New York Immigration Coalition.
Immigrant New Yorkers are under relentless attack from the anti-immigrant forces that wield the levers of control in Washington, DC. In this environment, it falls on New York State to devise solutions to the crisis. Access to health care represents a key element of immigrant inclusion and protection that state and local governments must address. In acknowledgment of the ongoing health access disadvantages that immigrants face and the acute needs related to the current sociopolitical dynamic, the New York State Assembly has called a public hearing on immigrant health for 10am on December 13. Public testimony is strongly encouraged from anyone with a stake in immigrant health access. The hearing will be held at 250 Broadway, New York, NY. This is the official Hearing Notice.
The hearing has been called by Assembly Health Committee Chair Richard Gottfried and cosponsored by New Americans Task Force Chair Michaelle Solages and Puerto Rican/Hispanic Task Force Chair Marcos Crespo. Coverage 4 All, a campaign of Health Care For All New York led by the New York Immigration Coalition and Make the Road New York, has been instrumental in advocating for the hearing. The campaign’s goal is to expand insurance eligibility to all New Yorkers to reduce disparities in coverage (noncitizens are five times more likely than citizens to be uninsured), but coverage is just one of the many current threats to immigrant health access:
- Persistent restrictions on health coverage based on immigration status, exacerbated by the Trump administration’s cancellation of many forms of immigration relief
- Pervasive fear of using health care services because of the dramatic increase in immigration enforcement and threats against immigrant communities
- Acute behavioral health care needs layered on a system that already cannot meet the demand for culturally and linguistically responsive behavioral health services
- Major cuts to uncompensated care funding that threaten the financial sustainability of safety-net health care systems
- Language access laws that lack sufficient monitoring and enforcement mechanisms
We strongly encourage testimony from anyone with a stake in immigrant health access – directly affected community members, concerned citizens, immigrant rights advocates, health care consumer advocates, health care providers, social services providers, legal services providers, local and state health officials, and faith communities, to name a few. This hearing is an unprecedented chance to voice concerns to the New York State Assembly, and to propose solutions the state can undertake to improve immigrant health access. Do not miss this opportunity!
NOTE: You must receive an invitation to testify. If you would like an invitation, please e-mail Claudia Calhoon of the New York Immigration Coalition at ccalhoon@nyic.org. If you are unable to attend the hearing in person, you are strongly encouraged to submit written testimony (the email for written submissions is included in the official Hearing Notice).

