There Are Still Huge Disparities in Federal Provider Relief Funding
Posted August, 12 2020 by Amanda Dunker
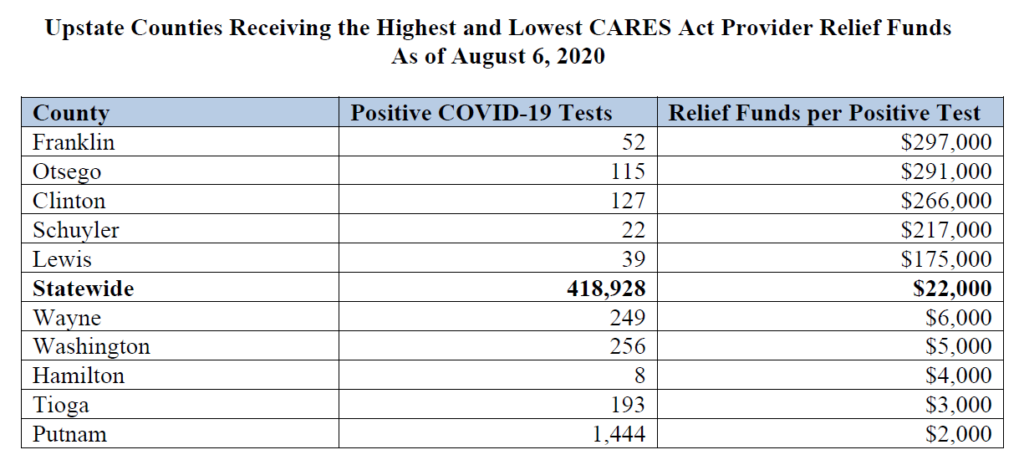
The Provider Relief Fund created by the Coronoavirus Aid, Relief, and Economic Security (CARES) Act is the biggest source of support for healthcare providers caring for COVID-19 patients. Yet, CARES Act disbursements vary enormously across New York, with little relationship to COVID-19’s burden. Providers in Putnam County, which has had around 1,400 confirmed COVID-19 cases, received the lowest funding: just $1,950 for each confirmed case. Franklin County, which received the highest funding, received $297,000 for each of its 52 confirmed cases. That’s 150 times higher! (Data on provider relief payments can be found here, and data on the number of COVID-19 cases by county here.)
The funding disparity also exists within New York City. Providers in Manhattan received over ten times as much relief funding as those in Queens compared by the number of confirmed cases.
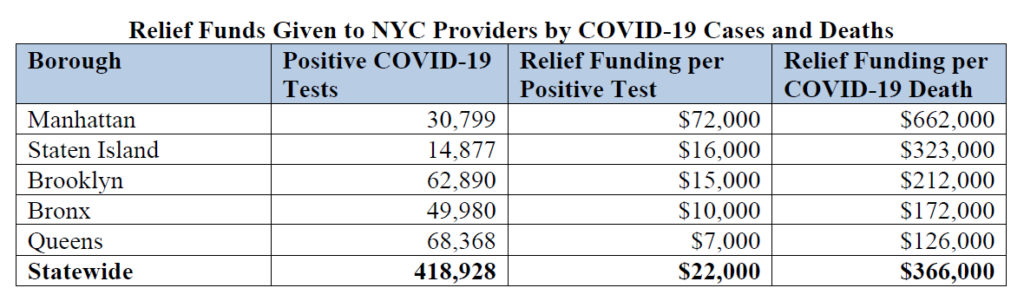
Sources: New York State Department of Health and the Centers for Disease Control.
Many of the positive cases identified outside of Manhattan may have resulted in care provided in Manhattan. Yet there is still a huge disparity when comparing the funding by the number of fatalities occurring in each borough, which would reflect differences in the burden experienced by providers. For every patient that died in Queens, providers there received about $126,000 in relief. In Manhattan, providers received $662,000 for every patient that died.
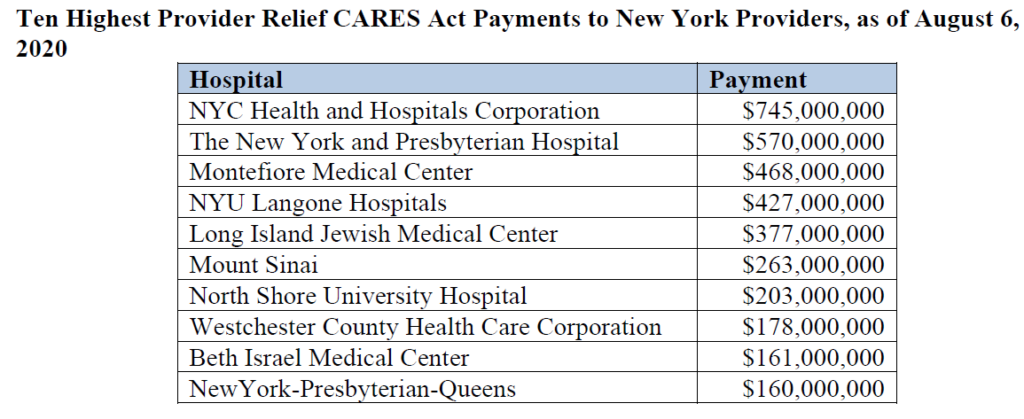
Troubling variation can also be seen at the provider level. The biggest payment, $745 million, went to the NYC Health and Hospitals Corporation. However, that system includes 11 different hospitals – which means it received just about $68 million for each facility. Other hospitals in the top ten appear to be individual facilities, and all received far more than $68 million. New York Presbyterian appears twice – it received $570 million for one of its hospitals in Manhattan and another $160 million for its hospital in Queens. Montefiore Medical Center received $468 million plus additional payments for its hospitals in New Rochelle and Mount Vernon.
Why has this happened?
Provider Relief funding is also meant to replace lost revenue so healthcare providers unable to see patients can stay open, and to cover the costs of testing and treatment for uninsured Americans. But it is still concerning that there is so little relationship between the impact COVID-19 had in different parts of the state and the amount of relief providers received.
The first Provider Relief disbursements were based on hospitals’ patient revenue – which guaranteed that safety-net providers (whose payer mix includes more uninsured patients and more patients covered by Medicaid) received far less funding. Later disbursements attempted to address the initial maldistribution. High Impact payments were distributed based on a threshold of COVID-19 admissions, meant to ensure at least $50,000 for every eligible admission. Another targeted disbursement went to hospitals with low profit margins or surpluses, uncompensated care costs of at least $25,000 per bed, and a Medicare Disproportionate Patient Percentage of at least 20.2 percent. However these additional targeted disbursements clearly fell short.
Federal funding disparities are just one of the reasons safety-net hospitals are under resourced. State policies such as the indigent care pool disbursements and our failure to reach universal health coverage also play a big role. Future relief packages must do something to get relief funding to providers caring for the highest number of COVID-19 patients.
